What You Need to Know About Your Gut microbiota and Your Metabolism: 5 Simple Ways Your Gut Bacteria Influences Your Metabolism
What You Need to Know About Your Gut microbiota and Your Metabolism: 5 Ways Your Gut Bacteria Influences Your Metabolism
Overview
Gut Microbiota and Metabolism – Have you ever wondered why some people seem to have a faster metabolism than others? Well, the answer might lie within your gut. Your gut is home to trillions of bacteria that make up your gut microbiota. Emerging research has shown that these tiny organisms play a crucial role in various aspects of our health, including metabolism. In this article, we will explore five fascinating ways in which your gut bacteria can influence your metabolism.
What types of bacteria are found in the gut?
The gut microbiota is composed of trillions of bacteria from various taxa. While it is difficult to provide an exhaustive list of all the bacteria found in the gut, here are some of the commonly identified types:
- Bacteroidetes: Bacteroidetes is a major phylum of bacteria found in the human gut. They are known for their ability to break down complex carbohydrates and fibers, producing short-chain fatty acids (SCFAs) as byproducts.
- Firmicutes: Firmicutes is another major phylum of bacteria in the gut. Some species within this phylum, such as Clostridium difficile, have been associated with obesity and metabolic disorders.
- Actinobacteria: Actinobacteria is a phylum of bacteria that includes the genus Bifidobacterium. Bifidobacteria are considered beneficial bacteria and are commonly found in the gut of healthy individuals. They are known for their ability to ferment dietary fibers and produce SCFAs.
- Proteobacteria: Proteobacteria is a diverse phylum that includes various bacteria, including Escherichia coli (E. coli). While some Proteobacteria species are beneficial, others can be pathogenic.
- Verrucomicrobia: Verrucomicrobia is a phylum of bacteria that includes the genus Akkermansia. Akkermansia muciniphila is a well-studied species within this genus that has been associated with a healthy gut and improved metabolic health.
It is important to note that the composition of the gut microbiota can vary greatly between individuals and can be influenced by factors such as diet, lifestyle, and overall health. A diverse and balanced gut microbiota, characterized by a variety of bacterial species, is generally considered beneficial for overall health and metabolic function.
What is metabolism?
Metabolism is a complex set of biochemical processes that occur within living organisms, including humans. It encompasses the conversion of food into energy, the synthesis and breakdown of molecules, and the regulation of various physiological functions. Here are some details and specifics about metabolism:
- Energy Metabolism: One of the primary functions of metabolism is to extract energy from the food we consume and convert it into a usable form, primarily in the form of adenosine triphosphate (ATP). The breakdown of macronutrients, such as carbohydrates, fats, and proteins, through processes like glycolysis, beta-oxidation, and the citric acid cycle, releases energy that is captured in ATP molecules.
- Anabolism and Catabolism: Metabolism consists of two interconnected processes: anabolism and catabolism. Anabolism refers to the synthesis of complex molecules from simpler ones, requiring energy. This process is involved in building and maintaining cellular structures, such as proteins, nucleic acids, and lipids. Catabolism, on the other hand, involves the breakdown of complex molecules into simpler ones, releasing energy.
- Metabolic Rate: Metabolic rate refers to the speed at which an organism carries out metabolic processes. It is influenced by various
factors, including age, sex, body composition, physical activity, and genetics. Basal metabolic rate (BMR) represents the energy expenditure at rest, necessary to maintain basic bodily functions like breathing, circulation, and cell repair. The metabolic rate can vary between individuals, affecting how efficiently they utilize energy.
- Regulation of Metabolism: Metabolism is tightly regulated to maintain homeostasis and adapt to changes in the environment. Hormones, such as insulin, glucagon, and thyroid hormones, play crucial roles in regulating metabolic processes. For example, insulin promotes the uptake and storage of glucose, while glucagon stimulates the release of stored glucose when energy demand is high. The endocrine system and the nervous system work together to coordinate metabolic activities.
- Metabolism and Body Composition: Metabolism influences body composition, including the ratio of lean body mass to fat mass. Lean muscle mass has a higher metabolic rate compared to fat tissue, meaning that individuals with a higher proportion of muscle tend to have a higher basal metabolic rate. Regular physical activity and strength training can help increase muscle mass and boost metabolism.
- Metabolism and Weight Management: Metabolism plays a role in weight management. While metabolism alone does not determine weight gain or loss, it can influence energy balance. If energy intake exceeds energy expenditure, the excess energy is stored as fat, leading to weight gain. On the other hand, if energy expenditure exceeds energy intake, the body taps into stored fat for energy, resulting in weight loss.
Understanding metabolism and its intricate processes is crucial for maintaining overall health and managing body weight. Various factors, including diet, physical activity, and the composition of the gut microbiota, can influence metabolic function and impact an individual’s overall well-being. Many diseases are now being linked to metabolic dysfunction including, cancer, cardiovascular diseases, and diabetes to name a few.
The result of poor metabolism

- Obesity: One of the most prevalent conditions associated with poor metabolism is obesity. Obesity occurs when there is an imbalance between energy intake and expenditure, leading to an excessive accumulation of fat tissue. Factors such as a sedentary lifestyle, poor diet, and genetic predisposition can contribute to poor metabolic regulation and promote weight gain. Obesity is a complex condition that increases the risk of numerous health problems, including cardiovascular disease, type 2 diabetes, and certain cancers.
- Type 2 Diabetes: Type 2 diabetes is characterized by insulin resistance, impaired glucose regulation, and elevated blood sugar levels. Poor metabolism plays a significant role in the development of type 2 diabetes. Insulin resistance occurs when cells fail to respond effectively to insulin, leading to reduced glucose uptake. Factors such as excess body weight, sedentary lifestyle, and unhealthy dietary habits can contribute to the development of insulin resistance and subsequent diabetes.
- Metabolic Syndrome: Metabolic syndrome is a cluster of conditions that occur together, including abdominal obesity, high blood pressure, elevated blood sugar levels, and abnormal cholesterol levels. These conditions increase the risk of cardiovascular disease, stroke, and type 2 diabetes. Poor metabolism, often associated with insulin resistance and obesity, underlies the development of metabolic syndrome.
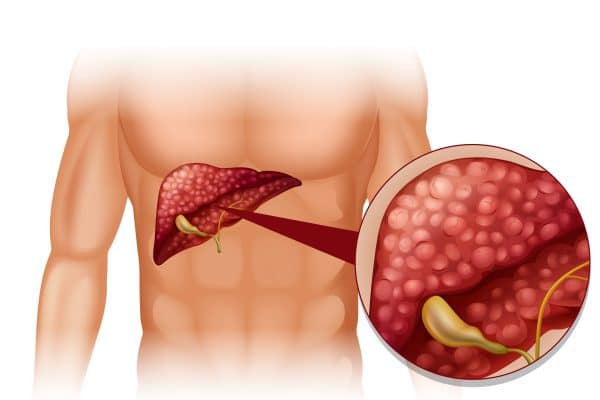
- Non-Alcoholic Fatty Liver Disease (NAFLD): Non-alcoholic fatty liver disease is characterized by the accumulation of fat in the liver in individuals who consume little to no alcohol. Poor metabolism, particularly abnormalities in lipid metabolism and insulin resistance, contribute to the development and progression of NAFLD. If left untreated, it can progress to more severe liver conditions, such as non-alcoholic steatohepatitis (NASH) and liver fibrosis.
- Cardiovascular Disease: Poor metabolism, specifically dyslipidemia (abnormal lipid levels) and insulin resistance, is closely associated with an increased risk of cardiovascular disease. Dyslipidemia, characterized by elevated levels of LDL cholesterol and reduced levels of HDL cholesterol, can contribute to the development of atherosclerosis and subsequent heart disease. Insulin resistance and the accompanying metabolic abnormalities further increase the risk of cardiovascular complications.
It’s important to note that poor metabolism is a complex issue influenced by various factors, including genetics, lifestyle, and environmental factors. Managing metabolic dysfunction often requires a comprehensive approach, including a healthy diet, regular physical activity, and medical interventions when necessary.
Please keep in mind that while I strive to provide accurate and up-to-date information, it is always recommended to consult with a healthcare professional for personalized advice and diagnosis.
How the Gut Influence Your Metabolism
Here are additional details and specific references for each of the five ways your gut bacteria influence your metabolism:
- Regulation of Energy Harvesting: Certain bacteria in your gut, such as Bacteroidetes and Firmicutes, are efficient at breaking down complex carbohydrates and fibers that are indigestible by human enzymes. This process produces short-chain fatty acids (SCFAs) as byproducts, which can be absorbed by the body and used as an additional energy source. A study by Sonnenburg and Bäckhed (2016) discusses the role of diet-microbiota interactions in modulating human metabolism.
- Appetite Regulation: The gut-brain axis is a communication pathway between the gut and the brain. Gut bacteria produce hormones and neurotransmitters that regulate appetite and satiety. For example, certain bacteria produce peptide YY (PYY), a hormone that helps reduce appetite, while others produce ghrelin, a hormone that stimulates hunger. Cani and Delzenne (2011) discuss the gut microbiota as a therapeutic target.
- Regulation of Fat Storage: Imbalances in the gut microbiota composition can contribute to obesity and affect the storage of excess calories as fat. Certain bacteria, such as Firmicutes, are associated with increased energy extraction from food and promoting fat storage. Additionally, the gut microbiota can influence the expression of genes related to fat storage and metabolism. Tremaroli and Bäckhed (2012) explore the functional interactions between the gut microbiota and host metabolism.
- Regulation of Insulin Sensitivity: The gut microbiota can impact insulin sensitivity, which plays a crucial role in glucose metabolism. Certain bacteria produce metabolites that can modulate insulin signaling pathways, affecting the body’s ability to utilize glucose effectively. Vrieze et al. (2012) conducted a study showing that transferring intestinal microbiota from lean donors increased insulin sensitivity in individuals with metabolic syndrome.
- Inflammation and Metabolic Disorders: Imbalances in the gut microbiota can lead to chronic low-grade inflammation, which is associated with various metabolic disorders, including obesity and metabolic syndrome. The gut microbiota influences inflammation levels throughout the body. Serino and Blasco-Baque (2021) discuss the complex relationship between the gut microbiota and inflammation.
These references provide more in-depth information on each aspect of how gut bacteria influence metabolism and offer insights into the scientific studies conducted in the field.
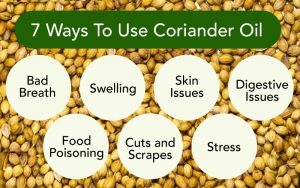
Natural ways to improve your gut microbiota and metabolism
Here are some natural strategies to improve your gut microbiota and metabolism:
- Eat a Diverse Diet: Consuming a wide variety of plant-based foods, such as fruits, vegetables, whole grains, legumes, and nuts, can enhance the diversity of your gut microbiota. These foods provide prebiotic fibers that serve as nourishment for beneficial bacteria. Aim to incorporate a rainbow of colors into your meals to ensure a range of nutrients and fiber.
- Probiotic and Fermented Foods: Include probiotic-rich foods in your diet, such as yogurt, kefir, sauerkraut, kimchi, and kombucha. These foods contain live beneficial bacteria that can help diversify and support a healthy gut microbiota. Fermented foods, in particular, provide a source of beneficial microbes and can enhance digestion and nutrient absorption.
- Reduce Sugar and Processed Foods: High intake of added sugars and processed foods can negatively impact the gut microbiota and metabolic health. These foods tend to be low in fiber and can promote the growth of less beneficial bacteria. Limiting the consumption of sugary drinks, sweets, refined grains, and processed snacks can support a healthier gut microbiota and metabolism.
- Regular Physical Activity: Engaging in regular exercise has been shown to have positive effects on the gut microbiota and metabolic health. Physical activity can increase microbial diversity, improve gut barrier function, and enhance insulin sensitivity. Aim for a combination of aerobic exercise and strength training for optimal benefits.
- Manage Stress: Chronic stress can disrupt the gut microbiota and metabolic function. Practice stress management techniques such as meditation, deep breathing exercises, yoga, or engaging in hobbies that promote relaxation. Prioritizing sleep and ensuring adequate rest is also essential for maintaining a healthy gut and metabolism.
Remember, these strategies should be implemented as part of a holistic approach to overall health. It’s always a good idea to consult with a healthcare professional or registered dietitian for personalized advice.
Final Thoughts
The influence of gut bacteria on metabolism is a fascinating area of research that is still being explored. The five ways discussed in this article highlight the importance of maintaining a healthy and diverse gut microbiota for optimal metabolic health. By nurturing your gut microbiota through a balanced diet, regular exercise, and other lifestyle factors, you can potentially optimize your metabolism and promote overall well-being.
For natural and healing remedies, products, and supplements that can help you live your most optimal healthy life, visit our store here!
To Your Health!
References
- Sonnenburg, J. L., & Bäckhed, F. (2016). Diet-microbiota interactions as moderators of human metabolism. Nature, 535(7610), 56-64.
- Cani, P. D., & Delzenne, N. M. (2011). The gut microbiome as therapeutic target. Pharmacology & Therapeutics, 130(2), 202-212.
- Tremaroli, V., & Bäckhed, F. (2012). Functional interactions between the gut microbiota and host metabolism. Nature, 489(7415), 242-249.
- Vrieze, A., Van Nood, E., Holleman, F., Salojärvi, J., Kootte, R. S., Bartelsman, J. F., … & Nieuwdorp, M. (2012). Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology, 143(4), 913-916.e7.
- Serino, M., & Blasco-Baque, V. (2021). Gut microbiota and inflammation: a complex relationship. Gut Microbes, 13(1), 1-12.
- Sender, R., Fuchs, S., & Milo, R. (2016). Revised estimates for the number of human and bacteria cells in the body. PLoS Biology, 14(8), e1002533.
- Qin, J., Li, R., Raes, J., Arumugam, M., Burgdorf, K. S., Manichanh, C., … & Wang, J. (2010). A human gut microbial gene catalogue established by metagenomic sequencing. Nature, 464(7285), 59-65.
- Cani, P. D., & Van Hul, M. (2020). Gut microbiota and obesity: benefits and pitfalls of association studies. Nature Reviews Endocrinology, 16(2), 59-66.
- Derrien, M., & Veiga, P. (2017). Rethinking diet to aid human-microbe symbiosis. Trends in Microbiology, 25(2), 100-112.
- Berg, J. M., Tymoczko, J. L., & Gatto, G. J. (2019). Stryer’s biochemistry. W.H. Freeman.
- Jitrapakdee, S., & Wallace, J. C. (2016). The biotin enzyme family: conserved structural motifs and domain rearrangements. Current Protein & Peptide Science, 17(4), 346-355.
- Bray, G. A., & Lovejoy, J. C. (2008). Definition and classification of the mechanisms of obesity. Gastroenterology, 134(5), 329-337.
- Westerterp, K. R. (2017). Exercise, energy expenditure and energy balance, as measured with doubly labeled water. Proceedings of the Nutrition Society, 76(4), 507-513.
- Eckel, R. H., Grundy, S. M., & Zimmet, P. Z. (2005). The metabolic syndrome. The Lancet, 365(9468), 1415-1428.
- Tilg, H., & Moschen, A. R. (2010). Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology, 52(5), 1836-1846.
- Alberti, K. G., Eckel, R. H., Grundy, S. M., Zimmet, P. Z., Cleeman, J. I., Donato, K. A., … & Smith, S. C. (2009). Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation, 120(16), 1640-1645.
- DeFronzo, R. A., & Ferrannini, E. (1991). Insulin resistance: a multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care, 14(3), 173-194.
- Haslam, D. W., & James, W. P. (2005). Obesity. The Lancet, 366(9492), 1197-1209.
- Dinan, T. G., Stilling, R. M., Stanton, C., & Cryan, J. F. (2015). Collective unconscious: how gut microbes shape human behavior. Journal of Psychiatric Research, 63, 1-9.
- Mailing, L. J., Allen, J. M., Buford, T. W., Fields, C. J., Woods, J. A., & Hand, G. A. (2019). Exercise and the gut microbiome: a review of the evidence, potential mechanisms, and implications for human health. Exercise and Sport Sciences Reviews, 47(2), 75-85.
- Malik, V. S., Li, Y., Pan, A., De Koning, L., & Hu, F. B. (2016). Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care, 38(4), 9-13.
- Marco, M. L., Heeney, D., Binda, S., Cifelli, C. J., Cotter, P. D., Foligne, B., … & Hill, C. (2021). Health benefits of fermented foods: microbiota and beyond. Current Opinion in Biotechnology, 70, 1-8.
- Sonnenburg, J. L., & Bäckhed, F. (2016). Diet-microbiota interactions as moderators of human metabolism. Nature, 535(7610), 56-64.






















1 Comment
[…] Symptoms of Nonalcoholic Fatty Liver Disease (NAFLD) and Alcoholic Liver Disease (ALD): […]